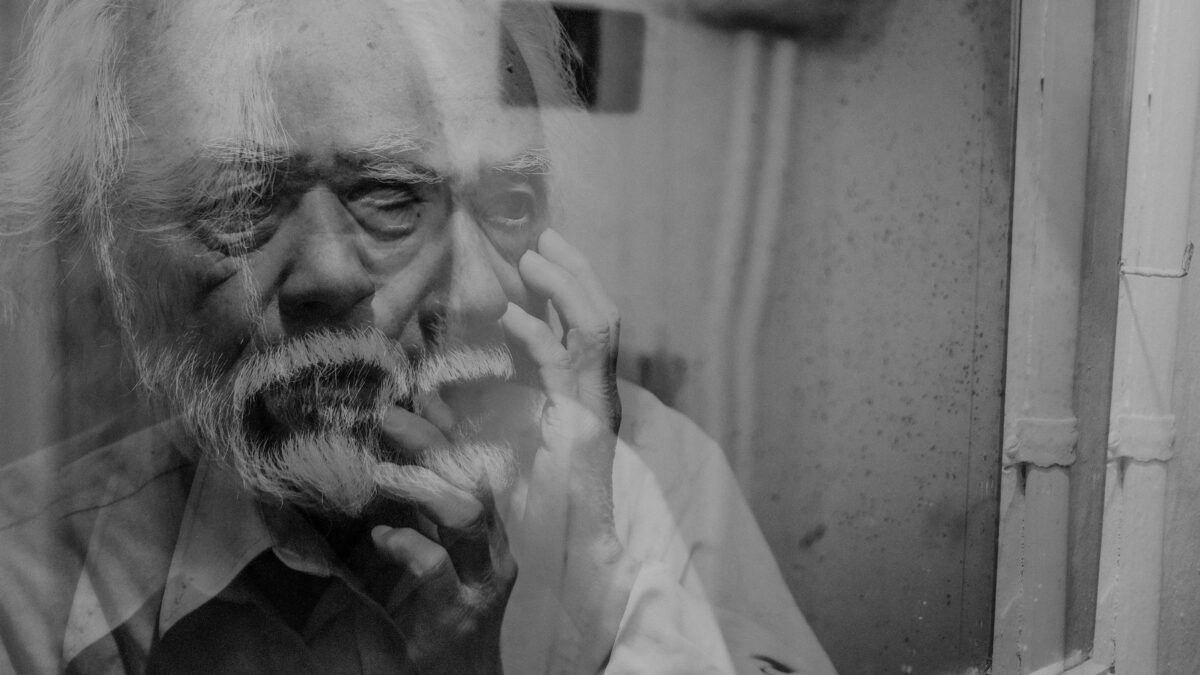
Dementia is a progressive neurological condition that profoundly affects cognitive functions, behavior, and daily living activities. Recognizing the 10 signs death is near dementia can be an emotional yet essential part of caregiving for someone in the final stages of this debilitating condition. Dementia, a progressive cognitive disorder, gradually strips away memory, communication, and independence. As the disease reaches its final phase, both physical and mental functions begin to decline rapidly, signaling that the end of life may be approaching. Comprehending these signs not only prepares families for what to expect but also helps guarantee that their loved one receives compassionate, dignified care during this delicate time.
Table of Contents
ToggleWhat Is Dementia?
Dementia is an umbrella term for a range of cognitive impairments characterized by a decline in memory, reasoning, communication, and the ability to perform everyday tasks. Alzheimer’s disease is the most prevalent form, but other types include vascular dementia, Lewy body dementia, and frontotemporal dementia. These conditions are typically irreversible and worsen over time, significantly impacting the individual’s quality of life.
Signs and Challenges of Dementia
As dementia progresses, individuals may experience:
Memory Loss: Difficulty recalling recent events, recognizing loved ones, or placing essential information.
Communication Difficulties: Struggles with finding the right words, following conversations, or expressing thoughts.
Disorientation: Confusion about time, place, or identity, leading to getting lost in familiar settings.
The Sun
Behavioral Changes: Mood swings, depression, anxiety, aggression, or apathy.
Physical Decline: Impaired coordination and mobility, increasing the risk of falls.
These challenges necessitate comprehensive care strategies to manage symptoms and support both the individual and their caregivers.
Psychological Perspective on Dementia
From a psychological standpoint, dementia not only affects cognitive functions but also has profound emotional and social implications. Individuals may experience frustration, fear, and sadness due to their declining abilities. Caregivers often face emotional stress, grief, and burnout. Psychological interventions concentrate on improving the quality of life through cognitive therapies, emotional support, and creating structured, familiar environments to reduce confusion and anxiety.
10 Signs Death Is Near in Dementia Patients

1. Significant Physical Weakness
In the final stages, individuals often exhibit profound physical debilitation. Simple tasks such as sitting up, holding objects, or moving limbs become increasingly challenging. This marked decline necessitates comprehensive assistance with all activities of daily living, including feeding, dressing, and personal hygiene. The pronounced frailty also heightens the risk of pressure sores and infections, requiring vigilant care and frequent repositioning to maintain comfort and prevent complications.
2. Severe Weight Loss
Dramatic and unintentional weight loss is common as dementia progresses. Factors contributing to this include a diminished sense of hunger and thirst, difficulties with chewing and swallowing, and metabolic changes. This substantial weight loss can lead to muscle wasting, decreased immunity, and increased vulnerability to infections. Nutritional support becomes critical, often involving modified diets or supplemental feeding to ensure adequate caloric intake and hydration.
3. Difficulty Swallowing (Dysphagia)
As neurological functions deteriorate, swallowing becomes impaired, posing significant risks such as choking and aspiration pneumonia. Careful assessment by speech and language therapists is essential to determine safe feeding techniques. In some cases, alternative feeding methods, like the use of feeding tubes, may be considered to maintain nutrition while minimizing risks.
4. Increased Susceptibility to Infections
The compromised immune system in late-stage dementia patients makes them more prone to infections, particularly urinary tract infections and pneumonia. These infections can exacerbate overall decline and often become life-threatening. Prompt identification and treatment are crucial, but the emphasis may shift towards palliative care to ensure comfort rather than aggressive interventions.
5. Incontinence
Loss of bladder and bowel control is prevalent due to the decline in neurological control over these functions. This incontinence necessitates meticulous hygiene practices to prevent skin breakdown and infections. The use of incontinence products and regular skin assessments becomes an integral component of care.
6. Communication Difficulties
Verbal communication may diminish significantly, with individuals speaking only a few words or becoming entirely nonverbal. Despite this, they may still respond to nonverbal cues such as touch, facial expressions, and tone of voice. Caregivers should focus on these forms of communication to provide comfort and reassurance, maintaining a connection despite the verbal limitations.
7. Altered Breathing Patterns
Irregularities in breathing, including periods of apnea (pauses in breathing) or Cheyne-Stokes respiration (a pattern of deep breathing followed by shallow breaths or pauses), are indicative of the body’s systems slowing down. These changes can be distressing to observe but are typically not uncomfortable for the patient. Providing a calm environment and positioning the patient to ease breathing can be beneficial.
8. Decreased Appetite and Thirst
A natural reduction in the desire to eat or drink occurs as the body’s need for energy diminishes. Forcing food or fluids can cause discomfort; thus, the emphasis should be on offering small sips of water or moistening the mouth to maintain comfort. This approach aligns with palliative care principles, focusing on quality of life rather than nutritional intake.
9. Increased Sleep and Unresponsiveness
Extended periods of sleep and reduced responsiveness are common as the body conserves energy. Individuals may become unresponsive to verbal stimuli but can often still hear. Speaking softly and providing a gentle touch can offer comfort, even if the individual does not outwardly respond.
10. Cold Extremities and Changes in Skin Color
As circulation diminishes, hands and feet may become cold to the touch, and skin may exhibit mottling or a bluish hue. These signs indicate that the body’s systems are shutting down.
Comprehending the 10 signs death is near dementia is a deeply emotional yet necessary step for families and caregivers guiding the final phase of a loved one’s life. While no two experiences are exactly the same, recognizing these signs allows for more informed decisions, greater emotional preparedness, and the ability to offer comfort and dignity in their last days. By being attentive, compassionate, and knowledgeable, we can honor their life with the peace and care they deserve, even in the quietest moments.
Watch and Read!
- “The 36-Hour Day” by Nancy L. Mace and Peter V. Rabins
- “Being Mortal” by Atul Gawande
- “Creating Moments of Joy Along the Alzheimer’s Journey” by Jolene Brackey
- “Still Alice” (2014)
- “Away From Her” (2007)
FAQs
The final stage of dementia can vary, typically lasting from several weeks to a few months. During this period, the person may become bedridden, unresponsive, and completely dependent on others for care. Palliative and hospice care are often introduced to provide comfort.
While some individuals may experience pain due to related conditions (e.g., infections, immobility), dementia itself does not directly cause pain. However, because communication is limited, it’s important to monitor non-verbal cues and provide appropriate pain relief.
Recognition often fades in advanced dementia, but some individuals may still respond to familiar voices, music, or physical touch. Emotional memory can linger even when cognitive recognition is lost.